Why Would My Baby Need MRI Brain Scans?
Magnetic Resonance Imaging (MRI) brain scans are images that are crucial for diagnosing and treating brain injuries in newborn babies. MRIs produce highly-detailed images, so they are the recommended method for newborn imaging.
Brain scans also help doctors assess a baby’s risk of having cognitive, developmental, or motor problems as they grow and develop. Doctors may use them to make predictions about the child’s long-term health. Quite frequently, however, the long-term effects of newborn brain damage related to cognitive abilities aren’t fully known until the child reaches school age and delays in their development become more obvious.
Did your baby need brain scans at birth?
We can review your child’s medical records for free to determine if negligence was a factor in their injuries.
Early scans are essential
A study published in The Journal of Pediatrics found that brain scans performed close to the baby’s birth are better predictors of neurodevelopmental outcomes than scans done later. The early scans are essential because they help detect conditions that need to be medically managed right away, such as brain bleeds, hypoxic-ischemic encephalopathy (HIE), or edema (swelling).
Brain imaging is also important for premature babies who are at risk for neurodevelopmental impairment. However, any baby suspected of having a brain injury during or near the time of birth must have brain scans performed on them to assess for injury.
Types of newborn brain imaging
- Magnetic resonance imaging (MRI): scanning technology that takes 3D images
- Cranial ultrasounds (CUS): use sound waves to produce images of the brain
- Computed tomography (CT): specialized x-rays that show internal organs, blood vessels, bones, and soft tissue
Magnetic resonance imaging (MRI) and cranial ultrasounds (CUS) are common head imaging techniques that give doctors pictures of the baby’s brain and determine if important structures are injured. MRI and CUS are often used together to diagnose injuries such as hypoxic-ischemic encephalopathy (HIE), brain bleeds, and hydrocephalus, which must be promptly treated.
MRIs produce highly-detailed images without exposing babies to ionizing radiation, so they are most recommended for newborn brain imaging. Cranial ultrasound is often used with other imaging options, since it produces a less clear and complete picture on its own. Likewise, compared to MRI, CT scans alone are also limited in their ability to accurately show a brain injury like HIE, but are sometimes better for showing hemorrhage.
Early intervention is critical for babies who experienced brain injuries and a lack of oxygen to the brain. The longer that a brain injury is left untreated, the higher the risk of permanent brain damage. However, because a newborn brain injury changes over hours, days, and weeks, multiple brain scans are sometimes done.
When Are Baby Brain Scans Performed?

Usually, brain injury in a newborn baby occurs during or close to the time of birth. Brain scans performed at different times are necessary to fully understand a birth injury, since the injury can evolve over time.
When doctors suspect a brain injury occurred, they will look for signs and symptoms of brain dysfunction, also known as neonatal encephalopathy. Signs and symptoms of brain injury are typically seen at 12 – 24 hours after birth, and brain swelling (edema) is usually evident at this time as well. When edema occurs in the first day or so after delivery, it is a strong indicator that the baby experienced a brain injury during or near the time of birth. An MRI can usually show moderate to severe forms of an injury like HIE within 24 hours of birth.
An MRI is best for assessing the extent of white matter brain damage, and it can usually show brain injury by day one of life, but MRIs are more typically performed at day 4 or 5 of life after cooling is performed. Once doctors identify a baby’s initial brain injury, brain scans should be done so they can evaluate how the brain injury changes. Sometimes, brain imaging is normal even when a baby has suffered a brain injury from not getting enough oxygen.
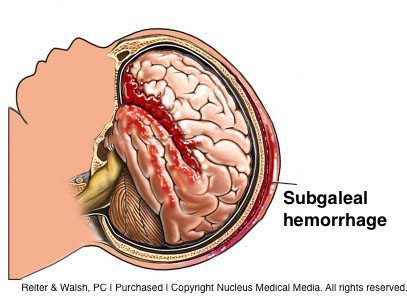
Baby brain bleeds (hemorrhages)
Brain bleeds (hemorrhages) in a baby can be diagnosed right away with cranial ultrasounds (CUS). Cranial ultrasounds can show images of the brain and surrounding areas, including the flow of blood to the baby’s brain.
An intraventricular hemorrhage (IVH) is a type of brain bleed that causes significant brain injury in premature babies. Most cases of IVH take place within the first five days after birth. Some occur and can be detected an hour after birth. A subdural hemorrhage is the most common type of intracranial hemorrhage in newborn babies. When a baby has symptoms of a subdural hemorrhage or hematoma, they usually occur within the first 24 – 48 hours of life.
When babies don’t show symptoms, a CUS performed for suspected head trauma or brain injury can easily detect this type of bleed. CUS helps the medical team determine the location and extent of brain bleeds in babies.
A subgaleal hemorrhage is one of the most serious types of brain bleeds in a baby and it is most frequently caused by a vacuum extraction or traumatic delivery. When a baby has a severe subgaleal hemorrhage, the head swelling may be evident right after birth, although swelling usually develops over a 12 – 72 hour period. Computed tomography (CT scans) and MRIs are useful for differentiating a subgaleal hemorrhage from other cranial medical conditions.
Intraventricular hemorrhages can also lead to hydrocephalus, or brain swelling. It’s caused by enlarged brain ventricles from problems with the flow of cerebral spinal fluid (CSF). In a newborn, CUS is used for the initial diagnosis of hydrocephalus, but an MRI can better show the extent of the condition, especially the CSF pathway. When a baby gets older and part of their soft spot closes, CUS can no longer be used, and CT or MRI must be performed for diagnosis and assessment of the baby’s hydrocephalus. Hydrocephalus may be present at or shortly after birth and must be quickly diagnosed and treated.
While these are critical examples, there are numerous conditions that can cause a baby to have brain damage. Prompt diagnosis of a brain injury is crucial so the medical team can intervene to minimize or prevent permanent brain damage in the baby.
Was your baby diagnosed with a brain injury?
Some brain injuries at birth are preventable. Call us to find out whether you have a legal case – absolutely free.
What Causes Brain Injuries In Babies?
Brain injuries in a baby can be caused by many factors and are classified into different types. One of the most common causes of brain injury in a baby is birth asphyxia, which is a lack of oxygen to the baby’s brain during or near the time of birth.
Types of birth asphyxia
Severe asphyxia is classified as either acute near-total asphyxia or acute-profound asphyxia. The first type usually causes injury to the deep gray matter of the brain, which affects many levels of the central nervous system. When the asphyxia is sudden and severe (acute near-total), deep structures in the brain, such as the basal ganglia, thalamus, and brain stem, are typically injured.
The following conditions can cause severe birth asphyxia in a newborn:
- Placental abruption
- Uterine rupture
- Prolapsed umbilical cord
- A very slow heart rate in the baby (bradycardia)
When the baby suffers asphyxia that is moderate to severe and relatively prolonged (acute-profound), injury will typically be seen in the cerebral cortex as well as the deep brain structures, particularly the putamen and thalamus.
Partial-prolonged asphyxia usually lasts for more than 30 minutes and it mainly causes injury in the watershed and parasagittal regions of the brain’s cortex, which are areas that do not have direct blood supply.
The conditions listed below can cause a baby to experience partial prolonged asphyxia:
- Use of the labor drugs Pitocin or Cytotec
- High blood pressure in the mother (hypertension)
- Low maternal blood pressure (hypotension), which can be caused by mismanaged anesthesia, maternal infection, or dehydration
- Umbilical cord compression caused by a nuchal cord (cord wrapped around baby’s neck)
- Oligohydramnios (low amniotic fluid)
- Placental insufficiency
- Inadequate or delayed resuscitation of the baby at birth
Babies can also experience both severe birth asphyxia and partial prolonged asphyxia, which is referred to as a mixed brain injury pattern.
Are Newborn Brain Injuries Preventable?
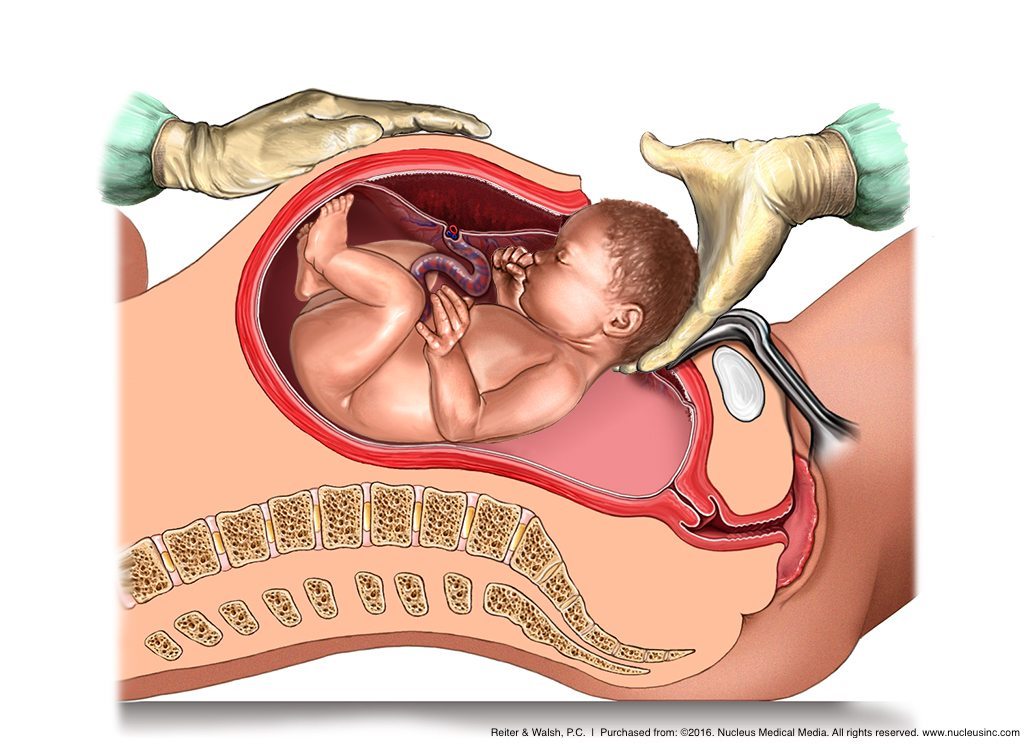
Yes, prompt delivery can prevent the baby from becoming injured. When a baby experiences an event that causes a lack of oxygen to their brain, the doctor should deliver right away via emergency C-section to minimize the time and severity of the asphyxia.
As soon as a mother is admitted to the labor and delivery unit, the baby’s heart rate should be monitored by a fetal heart rate monitor. If the baby starts to experience a lack of oxygen to their brain, the heart monitor will show non-reassuring tracings. The medical team must pay close attention to the tracings so they can intervene if the tracings become non-reassuring. Usually a prompt C-section delivery is the best intervention.


Legal Help for Babies with a Brain Injury
Birth injury cases are complex, both medically and legally. For the best case outcome for your child, it’s critical to find an attorney and a law firm that focus specifically on birth injury cases. At ABC Law Centers: Birth Injury Lawyers, our attorneys have focused their entire careers on this area of law. They consistently secure multi-million dollar settlements for our clients.
Contact us today to begin your free case review. We will answer your questions, help you understand where malpractice may have occurred in your child’s case, determine the negligent party, and explain your legal options. Moreover, you pay nothing throughout the entire legal process unless we win or favorably settle your case.
Featured Videos
Posterior Position
Hypoxic-Ischemic Encephalopathy (HIE)

Featured Testimonial
What Our
Clients Say…
After the traumatic birth of my son, I was left confused, afraid, and seeking answers. We needed someone we could trust and depend on. ABC Law Centers: Birth Injury Lawyers was just that.
- Michael
Helpful resources
- Hintz, Susan R., et al. “Neuroimaging and neurodevelopmental outcome in extremely preterm infants.” Pediatrics 135.1 (2015): e32-e42.
- Neuroimaging in the evaluation of neonatal encephalopathy l Pediatrics
- Neonatal encephalopathy and neurologic outcome, second edition. Report of the American College of Obstetricians and Gynecologists’ Task Force on Neonatal Encephalopathy l Obstet Gynecol
- Declining diagnosis of birth asphyxia in California: 1991-2000 l Pediatrics
- A systematic review of the role of intrapartum hypoxia-ischemia in the causation of neonatal encephalopathy l Am J Obstet Gynecol
- Birth asphyxia: incidence, clinical course and outcome in a Swedish population. Acta Paediatr
- Intrapartum-related neonatal encephalopathy incidence and impairment at regional and global levels for 2010 with trends from 1990 l Pediatr Res
- Neonatal encephalopathy following fetal distress. A clinical and electroencephalographic study. Arch Neurol
- Neonatal brain injury. N Engl J Med
- Neonatal encephalopathy or hypoxic-ischemic encephalopathy? Appropriate terminology matters. Pediatr Res
- Magnetic Resonance Imaging (MRI) | Boston Children’s Hospital
- Ultrasound Imaging l FDA
- Pediatric CT l Radiological Society of North America
- https://www.mayoclinic.org/diseases-conditions/cerebral-palsy/diagnosis-treatment/drc-20354005


