What is Neonatal Encephalopathy?
Neonatal encephalopathy (NE) is a broad term for neurological dysfunction in an infant. Neonatal encephalopathy can stem from a wide variety of causes (1). Oxygen deprivation at birth (birth asphyxia) is one of the most common causes of neonatal encephalopathy. Medical professionals may use the terms hypoxic-ischemic encephalopathy (HIE), perinatal asphyxia, intrapartum asphyxia, and birth asphyxia interchangeably with neonatal encephalopathy, even though they are slightly different conditions.
What is Neonatal Encephalopathy (NE)?
“Neonatal encephalopathy” encompasses any form of central nervous system dysfunction caused by an injury to the brain. This term is used when discussing injury in babies born at or later than 35 weeks of gestation (babies who are either late-preterm or term) (1, 2). Neonatal encephalopathy is estimated to occur in about two to nine of 1000 live births (2), and can be caused by numerous factors. These include the following (3):
- Birth asphyxia or hypoxic-ischemic encephalopathy (HIE)
- Meningoencephalitis (encephalitis with meningitis)
- Intracranial and extracranial hemorrhages (brain bleeds)
- Fetal stroke
- Infection
Conditions Associated with Neonatal Encephalopathy
Babies with neonatal encephalopathy or hypoxic-ischemic encephalopathy may have other related diagnoses, including:
- Brain damage
- Cerebral palsy
- Seizure disorders
- Hydrocephalus
- Periventricular leukomalacia (PVL)
- Microcephaly
What Does a Diagnosis of Neonatal Encephalopathy Mean?
A neonatal encephalopathy diagnosis can mean many things. At its simplest, it means that the baby has some degree of brain dysfunction. Sometimes, there is swelling inside the brain due to injury. In many cases, the baby ends up with no permanent damage or long-term consequences, especially if the encephalopathy is promptly recognized and treated.
Unfortunately, there are some cases in which the effects of neonatal encephalopathy are identified later on in life; when a child reaches four to five years of age and begins to miss major developmental milestones (4). Neonatal encephalopathy can lead to long-term conditions, such as cerebral palsy, developmental delays, or learning disabilities.
Signs and Symptoms of Neonatal Encephalopathy
Neonatal encephalopathy can be mild, moderate, or severe depending on its symptoms. Signs and symptoms of encephalopathy may include the following (2):
- Low Apgar scores
- A weak or absent cry at birth/delivery
- Seizures
- Require resuscitation
- An abnormal level of consciousness: Baby is hyperalert, irritable, lethargic, obtunded (not very alert).
- Tone and reflex abnormalities: Such as hypotonia (limp or floppy limbs) and/or hypertonia (stiff or spastic muscles).
- Absent primitive reflexes
- Apnea: Periods in which the baby stops breathing for 20 seconds or more.
- Feeding difficulties
- Respiratory problems
- Fever
- Neck stiffness: Common in cases of meningitis or meningoencephalitis.
- Hypotension
- Organ failure
- Hyper– or hypoglycemia
Newborn seizures are one of the most common signs of neonatal encephalopathy. It is important to note that seizures in babies do not look the same as seizures in adults; signs of seizures in babies are typically more subtle. Some babies with seizures have repetitive twitching or cycling motions in their limbs, or they may appear to stare blankly into space. These episodes can impact the baby‘s consciousness. These seizures must be quickly diagnosed via EEG testing and treated to prevent brain damage from worsening (5).
Treatment for Neonatal Encephalopathy
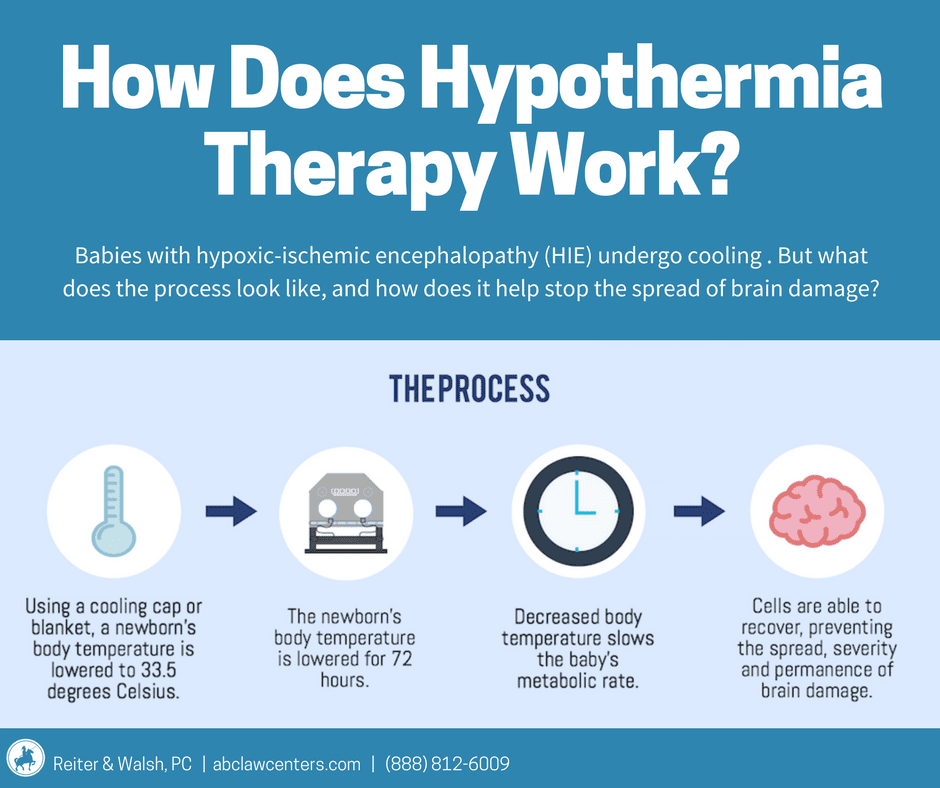
All moderate and severe instances of neonatal encephalopathy require treatment that takes place in the Neonatal Intensive Care Unit (NICU) (2). Because there are many different underlying mechanisms that can cause neonatal encephalopathy, managing and treating the injury is highly individualized. Some kinds of encephalopathy must be treated with therapeutic hypothermia (brain cooling) therapy. Not all types of encephalopathy are treated the same way, however. Encephalopathy caused by a bacteria or virus, for example, is treated by controlling the underlying infection. The key treatments include (2):
- Therapeutic hypothermia: Babies with hypoxic-ischemic encephalopathy should undergo therapeutic hypothermia within six hours of birth, lasting for a total of 72 hours (6).
- Ventilation: Babies with encephalopathy due to respiratory issues may be placed on a ventilator to help regulate their breathing and ensure adequate oxygenation. Medical professionals should avoid hyperoxia and hypoxemia (too much or too little oxygen).
- Seizures: Part of the treatment for neonatal encephalopathy is control of seizures. Certain medications can be used to treat seizures. Additionally, EEG monitoring should be used to monitor seizures regularly.
- Blood-related treatment: Babies with brain bleeds may be given blood products (such as packed red blood cells and fresh frozen plasma) or normal saline to correct blood pressure issues. Brain and organ perfusion should be maintained and hypertension, hypotension, and hyperviscosity avoided.
- IV: Babies experiencing strokes may be given IV fluids and medication to prevent blood clotting issues.
- Medication: Babies with encephalopathy due to infection may be given antiviral medication or antibiotics to control the infection (depending on infection type).
Causes of Neonatal Encephalopathy
Neonatal encephalopathy can be caused by a wide variety of complications during or around the time of birth, including the following.
Birth Asphyxia (lack of Oxygen to The Brain)
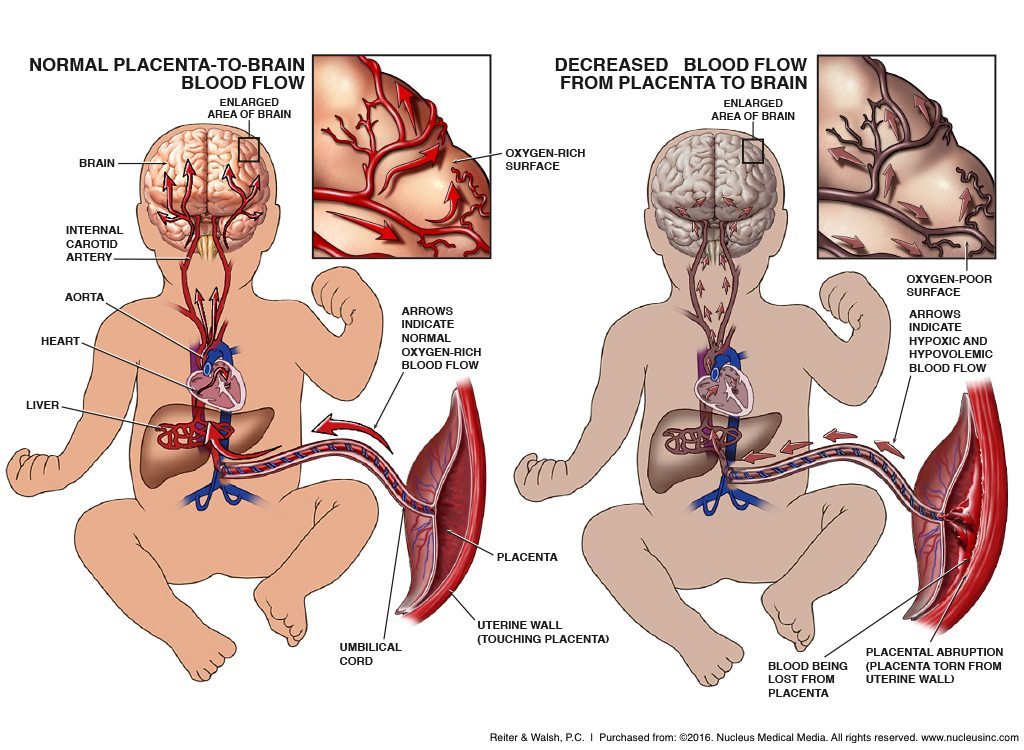
In the womb, babies get oxygen from the blood that travels from the mother to the placenta to the umbilical cord. Anything that interferes with this pathway can cause the baby to be deprived of oxygen (7). Some examples of causes of birth asphyxia include:
| Conditions that can cause neonatal encephalopathy (NE) due to hypoxia-ischemia | ||
| Placental insufficiency | Preeclampsia | Placental abruption |
| Uterine rupture | Umbilical cord prolapse | Nuchal cord(cord wrapped around baby’s neck) |
| Short umbilical cord | Umbilical cord in a true knot | Placenta previa |
| Stroke | Premature rupture of the membranes (PROM) | Prolonged and arrested labor |
| Oligohydramnios(low amniotic fluid) | Failure to quickly deliver the baby whenfetal distressis evident on the heart rate monitor | Hyperstimulation of the uterus caused by the labor induction drugs Pitocin, and Cervidil |
| Brain bleeds | Traumatic delivery | The use of forceps and vacuum extractors |
| Nuchal cord | Vasa previa | Post-term pregnancy |
Underlying Maternal Health Conditions
Certain health conditions can make a pregnancy high-risk. These health conditions carry with them a higher risk of birth injury, necessitating closer monitoring and more frequent prenatal care appointments. These conditions include (8):
| Conditions that can cause neonatal encephalopathy (NE) due to underlying maternal health conditions | ||
| Condition | Why? | |
| Gestational diabetes | Gestational diabetes → increased risk of preeclampsia → increased risk of placental abruption | |
| Maternal high blood pressure (preeclampsia) | Preeclampsia impacts blood flow through the placenta → baby may have poor oxygen or nutrient supply → baby may have poor growth/IUGR, which makes them more susceptible to neonatal encephalopathyIncreased risk of placental abruption → placental abruption can compromise blood and oxygen supply to baby | |
| Placental insufficiency | Can cause intrauterine growth restriction (IUGR) → baby can have potentially reduced oxygen reserves and cannot tolerate labor as well | |
| Oligohydramnios | Can cause intrauterine growth restriction (IUGR) → baby can have potentially reduced oxygen reserves and cannot tolerate labor as well | |
| Maternal Infections (such as Group B streptococcus (GBS), Chorioamnionitis, herpes simplex virus (HSV), E coli, Staphylococcus (staph)) | Infections can be passed to the baby during labor/delivery → can spread to become pneumonia, meningitis, encephalitis, or sepsis, causing seizures and brain damage | |
Traumatic Birth
It is very important that babies be delivered by experienced obstetricians, gynecologists or other medical staff who have proper knowledge of delivery techniques and procedures for difficult deliveries. If medical staff deliver the baby in a way that is not up to the standards of care, the baby can have a traumatic birth (8). The impact of a traumatic birth isn’t always immediately obvious – there may not be any external bleeding. Sometimes there will be internal bleeding (brain bleeds). Babies may show signs of neurological dysfunction immediately – in the form of seizures, for example – or – in some cases – the child will only show neurological dysfunction as they grow and begin missing major developmental milestones. Causes of traumatic birth can include:
| Causes of Traumatic Birth and Brain Bleeds | ||
| Misuse of vacuum extractors and forceps | Mismanaged delivery of a baby in breech position | Mismanaged delivery of a baby who is large for gestational age (macrosomic) |
| Mismanaged cephalopelvic disproportion (CPD) | Prolonged labor and uterine hyperstimulation | Trauma from abnormal changes in blood pressure |
Preventing Neonatal Encephalopathy (NE)
Many of the conditions that cause neonatal encephalopathy (NE) have known risk factors. This means that medical staff can prevent adverse outcomes by properly monitoring the mother’s and baby’s health and conducting interventions if necessary.
Many of these events affect the baby during labor and delivery. Because of the risks associated with labor and delivery, the baby’s heart rate should be continuously monitored with a fetal heart rate monitor (9). This monitor will alert the medical team if the baby starts to become oxygen-deprived, which will show up as a non-reassuring heart tracing (fetal distress). If fetal distress occurs, the physician should deliver the baby right away, often by C-section (the fastest and safest way to deliver a baby in distress).
One of the key things that is very important in preventing neonatal encephalopathy in babies is proper technique for using vacuum extractors or forceps if it becomes necessary. There should be no twisting of the head or neck, no excessive pulling, and no pulling for more than 20 minutes (10). If the vacuum extractor comes off 3 times during use, the physician should move on to a C-section (11). These instruments should only be used by physicians who follow standards of care, which includes being skilled.
If a baby has a brain bleed from a labor and delivery incident, the bleed must be promptly recognized and treated so that encephalitis and permanent conditions such as cerebral palsy can be avoided. This can include:
- Medications to help stop or slow the bleeding
- Medications to increase blood pressure and blood volume
- Ventilatory support for the baby (a breathing machine)
- Medications to decrease inflammation
- Close monitoring of intracranial blood pressure
Pregnant women are supposed to have regular prenatal check-ups that assess both their health and their baby’s health. Prenatal tests include non-stress tests and biophysical profiles (BPPs). If the mother has a high risk pregnancy, prenatal testing should be more frequent and she should be referred to a maternal-fetal specialist. These prenatal tests, when done properly, can detect underlying health conditions that can mean that a baby is at higher risk for having a birth injury.
During prenatal visits, physicians should pay close attention to test results, especially the baby’s heart tracings. These tracings, along with ultrasound results, will alert the medical team to health problems the baby may have, including if the baby is being deprived of oxygen. If this is occurring, the mother may be admitted to the hospital so the medical team can closely monitor the baby. Sometimes a baby may have to be delivered early to help prevent permanent brain damage from a lack of oxygen and/or nutrients.