Birth Asphyxia and HIE (Hypoxic Ischemic Encephalopathy) from Prolonged Labor
What happens if the baby is in the birth canal for too long?
If the baby is in the birth canal for too long, the baby may be in danger of oxygen deprivation. During each contraction, pressure is put on the blood vessels that provide the baby with oxygen and nutrients. If these blood vessels are squeezed for too long, the baby stops receiving oxygen-rich blood.
If the baby shows signs of distress during a prolonged labor, medical staff needs to intervene in time and deliver the baby by C-section.
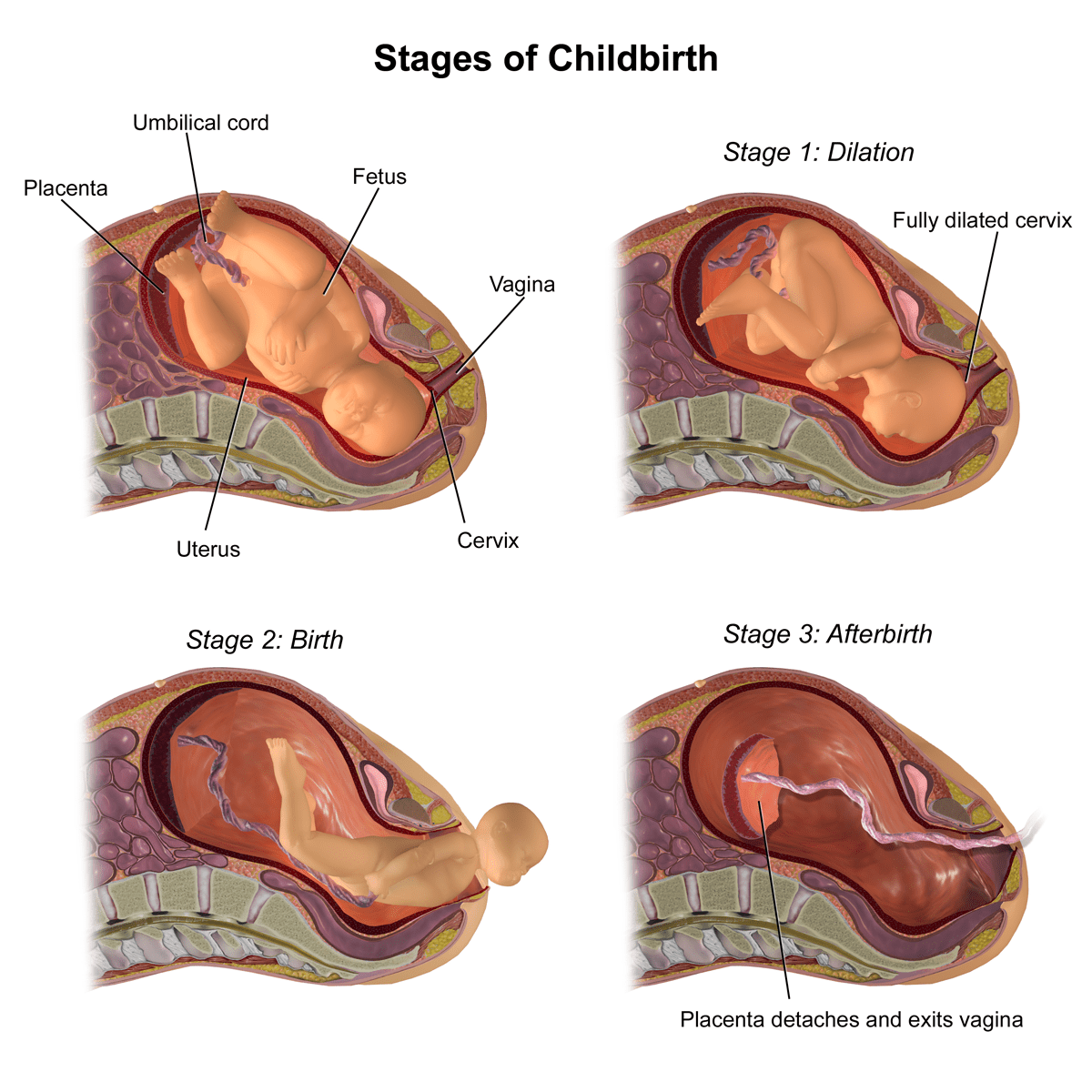
One form of prolonged labor is when the second stage of labor is going too long without progress. The second stage of labor starts when the cervix is fully dilated.
Because each patient is different, the amount of time to declare a failure to progress varies. ACOG and SMFM have general guidelines for determining prolonged labor. A first-time parent’s labor is considered prolonged after 3-4 hours of pushing. For a patient who has had a baby before, the second stage is considered prolonged after 2-3 hours.
However, clinicians should monitor patients and babies closely during labor to determine when intervention is needed. Many other factors may affect labor time, including the patient’s history, the size and weight of the baby, and the baby’s presentation.
If physicians do not properly manage prolonged labor, the baby can suffer serious complications, including birth asphyxia or hypoxic-ischemic encephalopathy (HIE).
A birth injury diagnosis after a prolonged labor is hard on your whole family. At ABC Law Centers, our attorneys focus only on families like yours. If you have any questions about your child’s HIE or birth injury diagnosis, call us for a free consultation today.
Birth Asphyxia and HIE: Definitions
Birth asphyxia occurs when a baby experiences a lack of oxygen to his or her brain during or near the time of birth.
Hypoxic ischemic encephalopathy (HIE) is a brain injury caused by insufficient oxygen in the blood and decreased blood flow in the brain.
Birth asphyxia and HIE can cause a baby to have permanent brain damage that may result in long-term conditions such as:
Birth asphyxia and HIE can often be prevented by closely monitoring the baby and quickly delivering her at the first signs of distress or impending distress. Skilled members of the medical team will be aware of distress if they continuously review the baby’s heart tracings on the fetal heart rate monitor. In addition, certain conditions make distress likely, and the medical team should monitor the mother and baby for these risky situations.
Birth asphyxia and HIE can cause severe birth injuries. In these situations, prolonged labor and obstructed labor often occur because health professionals lack the skills to prevent the injuries.
How Does Prolonged Labor Cause Birth Asphyxia and HIE (Hypoxic Ischemic Encephalopathy)?
Babies that go through a prolonged or arrested labor may start to experience birth asphyxia and HIE. The oxygen deprivation is due to umbilical cord problems or the stress of too many contractions.
Labor is usually considered prolonged when the first and second stages of labor combined are greater than 20 hours for a first pregnancy and greater than 14 hours for women with prior births.
Prolonged and arrested labor basically have 2 causes: inadequate contractions and/or mechanical impediments, like:
- Cephalopelvic disproportion (CPD)
- The baby’s head is larger than the birth canal
- Abnormal presentation
- Breech presentation
- Face presentation
- Brow presentation
- Shoulder presentation (transverse lie)
- Occipitoposterior (OP) position
- Limb presentation
- Compound presentation
Abnormal presentations and CPD increase the risk of numerous complications. These events increase the likelihood that the physician will attempt to speed up delivery by using labor drugs like Pitocin and Cytotec or delivery devices like vacuums and forceps. Often, these drugs and devices actually prolong labor and delivery. The physician relies on them instead of moving on to a prompt C-section delivery.
It is dangerous to force a vaginal delivery when CPD and certain breech positions occur.
Tell us your story.
Call ABC Law Centers: Birth Injury Lawyers today to secure your child’s care and reclaim their future.
Inadequate Uterine Activity or Inadequate Contractions
Inadequate uterine activity is sometimes a cause of prolonged and arrested labor. It refers to uterine activity that is either not strong enough or not appropriately coordinated to dilate the cervix and expel the baby. The uterine muscle may fail to properly contract when it is stretched, as in twin pregnancy and hydramnios (excess amniotic fluid). Tumors in the uterine musculature can also affect uterine contraction.
Uterine Stimulation with Pitocin or Cytotec
Inadequate contractions are usually treated with uterine stimulation through drugs like Pitocin or Cytotec. These drugs can cause excessive contractions, called hyperstimulation, which can injure the baby.
When contractions are too fast and strong, the placenta cannot provide oxygen-rich blood to the baby. The excessive contractions do not allow the placenta to recharge with an adequate supply of this blood for the baby. As hyperstimulation/tachysystole continues, the baby’s oxygen deprivation gets progressively worse.
Use of Pitocin or Cytotec requires very close monitoring of the baby’s heart rate, and the baby must be quickly delivered at the first signs of distress.
Inadequate Uterine Activity due to Painkillers or Anesthesia
Use of painkillers or anesthesia can sometimes cause inefficient uterine activity. These treatments may hinder pushing efforts by the mother to deliver the baby during the second stage of labor. Research shows that anesthesia can increase the length of the second stage of labor, and that it increases the use of Pitocin, as well as the frequency of forceps and vacuum extractor use.
Cervical Dystocia
The term cervical dystocia is used when the cervix fails to dilate properly and remains at the same position for more than 2 hours after the latent phase of labor. The cervix may fail to dilate when it is fibrosed due to previous operations, such as cone biopsy (type of cervical biopsy where a cone-shaped piece of tissue is removed), or due to the presence of tumors.
Physicians should be aware of these problems in a mother and should expect the possibility of a prolonged or arrested labor and the need for a prompt C-section delivery.
Preventing Birth Asphyxia and HIE (Hypoxic-Ischemic Encephalopathy)
Prevention of birth asphyxia and HIE (hypoxic ischemic encephalopathy) boils down to two major factors:
- Closely monitoring the mother and baby so that fetal distress or impending distress is recognized
- Quickly delivering the baby when fetal distress or impending distress are present.
During pregnancy, the mother and baby should have regular prenatal tests to help ensure fetal health. If the pregnancy is high risk, more frequent prenatal testing is required and the mother should be referred to a maternal-fetal specialist. Regular assessments like these can help clinicians determine their expectations for labor and delivery.
As soon as the mother is admitted to the labor and delivery unit, a fetal heart monitor should be attached to her body and the baby’s heart rate should be continuously monitored. The point of a fetal heart monitor is to alert the medical team of fetal distress. If the baby is experiencing a lack of oxygen to her brain, this will result in nonreassuring heart tracings on the fetal monitor.
In the event of fetal distress or other fetal emergencies, medical staff should prepare for a C-section delivery. Babies experiencing fetal distress or lack of oxygen during a prolonged labor must often be delivered within a matter of minutes.
Our team can help.
Secure your child’s future. Call the trusted birth injury attorneys at ABC Law Centers: Birth Injury Lawyers now.
How Can Prolonged Labor Cause Brain Damage, Cerebral Palsy, and Lifelong Disabilities?
When the brain goes without oxygen for too long, brain cells become injured. A cycle of injury starts to occur that can cause permanent brain damage. Birth asphyxia and HIE / hypoxic ischemic encephalopathy can cause the following conditions:


Legal Help for Children with Birth Injuries, Birth Asphyxia and HIE | Michigan Hypoxic Ischemic Encephalopathy Lawyers
If you are seeking the help of a lawyer, it is very important to choose a lawyer and firm that focus solely on birth injury cases. ABC Law Centers: Birth Injury Lawyers is a national birth injury law firm that has been helping children with birth injuries for over 3 decades.
If your child was diagnosed with a birth injury, such as cerebral palsy, a seizure disorder, or hypoxic ischemic encephalopathy (HIE), the award winning birth injury lawyers at ABC Law Centers: Birth Injury Lawyers can help.
We have helped children throughout the country obtain compensation for lifelong treatment, therapy and a secure future, and we give personal attention to each child and family we represent. Our nationally recognized birth injury firm has numerous multi-million dollar verdicts and settlements that attest to our success. No fees are ever paid to our firm unless we win your case.
Our team is available 24/7 to speak with you. Set up a free consultation with us today.
Featured Videos
Posterior Position
Hypoxic-Ischemic Encephalopathy (HIE)

Featured Testimonial
What Our
Clients Say…
After the traumatic birth of my son, I was left confused, afraid, and seeking answers. We needed someone we could trust and depend on. ABC Law Centers: Birth Injury Lawyers was just that.
- Michael
Helpful resources
- UpToDate | Labor: Diagnosis and Management of a prolonged second stage.
- Cleveland Clinic | Prolonged Labor (Failure to Progress)
- Executive summary: Neonatal encephalopathy and neurologic outcome, second edition. Report of the American College of Obstetricians and Gynecologists’ Task Force on Neonatal Encephalopathy. Obstet Gynecol 2014; 123:896.
- Wu YW, Backstrand KH, Zhao S, et al. Declining diagnosis of birth asphyxia in California: 1991-2000. Pediatrics 2004; 114:1584.
- Graham EM, Ruis KA, Hartman AL, et al. A systematic review of the role of intrapartum hypoxia-ischemia in the causation of neonatal encephalopathy. Am J Obstet Gynecol 2008; 199:587.
- Thornberg E, Thiringer K, Odeback A, Milsom I. Birth asphyxia: incidence, clinical course and outcome in a Swedish population. Acta Paediatr 1995; 84:927.
- Lee AC, Kozuki N, Blencowe H, et al. Intrapartum-related neonatal encephalopathy incidence and impairment at regional and global levels for 2010 with trends from 1990. Pediatr Res 2013; 74 Suppl 1:50.
- Chau V, Poskitt KJ, Miller SP. Advanced neuroimaging techniques for the term newborn with encephalopathy. Pediatr Neurol 2009; 40:181.


