Neonatal Imaging
Neonatal imaging is a process used to produce images of a newborn baby’s internal systems. Medical professionals use neonatal imaging to evaluate and diagnose many neonatal injuries, including hypoxic-ischemic encephalopathy (HIE), cerebral palsy, and intracranial hemorrhages. There are a few different forms of neonatal imaging, each with their own set of functions.

Magnetic resonance imaging (MRI)
An MRI is a form of non-invasive scanning technology that takes three-dimensional images of the body, without using radiation. In order to obtain an MRI, a patient must lie completely still inside of a magnetic machine. The magnets force protons in the body to align and then administer a radiofrequency current, which will pull them out of equilibrium. Then the radio frequency is turned off and the machine detects the energy released as the protons return to equilibrium (1). MRIs produce highly-detailed images, so they are the method most commonly recommended for neonatal imaging (2).

What are MRIs used for?
MRIs are useful for imaging:
- Non-bony parts of the body, including the brain, spinal cord, and nerves
- Contrasts in soft tissues, which helps them to diagnose infections, inflammatory conditions, tumors, problems with joints, cartilage, ligaments, and tendons, and other conditions or injuries.
- Abnormalities in the brain caused by brain damage that can cause neonatal seizures (3).
Why do some babies receive MRIs?
MRIs can be used to help diagnose neonatal injuries such as hypoxic ischemic encephalopathy (HIE), intracranial hemorrhages, hydrocephalus, white matter brain damage, and cerebral palsy.
Preparing for a baby's MRI
Sedation: In order to achieve successful imaging from an MRI, the patient must remain still in the MRI machine. This means that the majority of MRIs given to infants are administered using anesthesia. Anesthesia helps the child to go to sleep and remain motionless during the procedure. Food and drink will be stopped at some point before the MRI so that the infant is sedated on an empty stomach. It is important that the MRI technician be notified of previous drug reactions, allergies, or illnesses. If a child was recently ill or is getting sick, this should be mentioned to the doctor because they may recommend that the test be rescheduled. If the child is sedated, they will be monitored at all times during the test by a machine that detects oxygen level, heart rate, and breathing (4 5).
Removal of Metals: Any metallic objects must be removed before the infant gets an MRI. The doctor will also ask you questions to determine if your baby has any internal metal clips from a previous surgery or anything else that may cause a problem near a strong magnetic machine (4, 5).
Positioning: The infant will be placed on the scanning bed and then they will be positioned in the machine so that the area being imaged is in the center of the machine (2).
Comforts: Your child may be given headphones or earplugs to block out the noise from the machine. There will be a call button available so they can call if they become nervous during the test (4).
Company: Parents can stay in the MRI room with the child until the test begins. An MRI technician will perform the scan and the anesthesia team will be there to monitor (4).
Time: An MRI usually takes between 20 and 90 minutes to perform, depending on the type of images the technicians are looking for. Each scan will take a few minutes and then the infant will be moved out of the machine and repositioned for the next scan (2).
Afterwards: Following the MRI scan, your child she appear normal and happy. The contrast material should pass through the system within about 24 hours and the sedation should wear off within 1-2 hours (4).
Results: The radiologist will interpret the scans and send a report back to the infant’s doctor, who will then discuss the results with the parents (2).
Neonatal anesthesia
Neonatal anesthesia comes with its own set of limitations, which physicians will often counsel parents on before anesthesia administration. These limitations may include:
- A drug-induced depression of consciousness, with potential for loss of protective reflexes.
- Cardiorespiratory depression, which can include hypoventilation, hypoxia, and hypotension.
- Post-sedation side effects such as nausea, vomiting, disorientation, or sleep disturbances.
Contrast materials
Your doctor may recommend the use of contrast materials during certain imaging techniques, such as an MRI or CT scan. Contrast materials are dyes that are ingested to highlight certain parts of the body during the imaging test. They may be given by mouth, by enema, or by injection. Contrast materials can cause allergic reactions, so always check with your doctor before the child receives them. Medical staff that are prepared to deal with allergic reactions should be present during the scans. Parents should also mention if the child has any illnesses, drug reactions, or decreased kidney function, because these can cause complications when using contrast materials (4,5).
Benefits of magnetic resonance imaging (MRI)
- No radiation
- Presents a very clear and complete image
- Suitable for many scans in a row
- Can be used in conjunction with magnetic resonance spectroscopy to understand biochemical and physiological changes, in addition to structural imaging
Limitations of magnetic resonance imaging
- Often must be completed in a separate room, though new MRIs can be used in the NICU
- Expensive
Computed tomography (CT)
A CT scan uses a computerized x-ray machine to collect a series of images from a patient. These images are taken from different angles and then combined to create a three-dimensional picture of the area of interest (6).
What are CT scans used for?
CT scans are used to create detailed images of an infant’s blood vessels, organs, bones, and soft tissues. They are often used with infants to evaluate for injury after trauma or diagnose abdominal pain. They are especially useful in children for obtaining detailed images of the heart and blood vessels, and they are the second-most common method for obtaining images of the chest (the first being chest x-rays). These images can help diagnose pneumonia, tumors in the lungs, trauma to the lungs, birth defects, and other conditions (6,7).
Preparing for a neonatal CT
Sedation: Similar to the MRI, doctors may recommend an infant be given anesthesia before having a CT scan to keep them from moving around too much. Food and drink will be stopped at some point before the CT so that the infant is sedated on an empty stomach. It is important that the CT technician be notified of previous drug reactions, allergies, or illnesses. If a child was recently ill or is getting sick, this should be mentioned to the doctor because they may recommend that the test be rescheduled. If the child is sedated, they will be monitored at all times during the test by a machine that detects oxygen level, heart rate, and breathing (6).
Clothing: The infant should wear comfortable clothing during the exam (7).
Removal of Metals: Usually metallic objects will be removed before the infant gets a CT scan. The doctor may also ask questions to determine if the baby has any internal metal clips from a previous surgery or anything else that may cause a problem near the CT machine (7).
Positioning: The technician will position the child on the table such that the highest-quality images of the body parts in question can be obtained. Once the child is in the correct position, the technician will go into the adjacent room and begin the scan. The technician will always be watching the child through a window. The child will move through the machine while it takes the scans (6,7).
Breathing: If the CT machine is taking images of the chest, the doctor would ask an older child or adult to hold their breath. Infants will not be expected to do this (7).
Afterwards: After the CT scan, the child should be able to return to normal activities. If they received sedation, they will continue to be monitored for the effects of sedation and to note when it has worn off (7).
Results: The radiologist will interpret the scans and send a report back to the infant’s doctor, who will then discuss the results with the parents (7).
Benefits of computed tomography
- Available in many hospitals
- Relatively cheap
- Images can be stacked to achieve a complete three-dimensional picture
Limitations of computed tomography
- Use of ionizing radiation
- Must be completed in a separate room, often quite a distance from the NICU
- Not suitable for many scans in a row
- Not as accurate as MRI in terms of diagnosis of HIE
Ultrasound
An ultrasound is a non-invasive imaging technique that scans the inside of the body using ultrasound probes or cell transducers. Diagnostic ultrasound probes are normally placed on the skin with a gel substance between them, but they can also be placed inside the body for higher image quality. The transducers send out beams of sound waves into the body and these waves are reflected back by boundaries between tissues in their path. The machine is able to calculate the distance between the transducer and the tissue boundary, which creates an image (8).
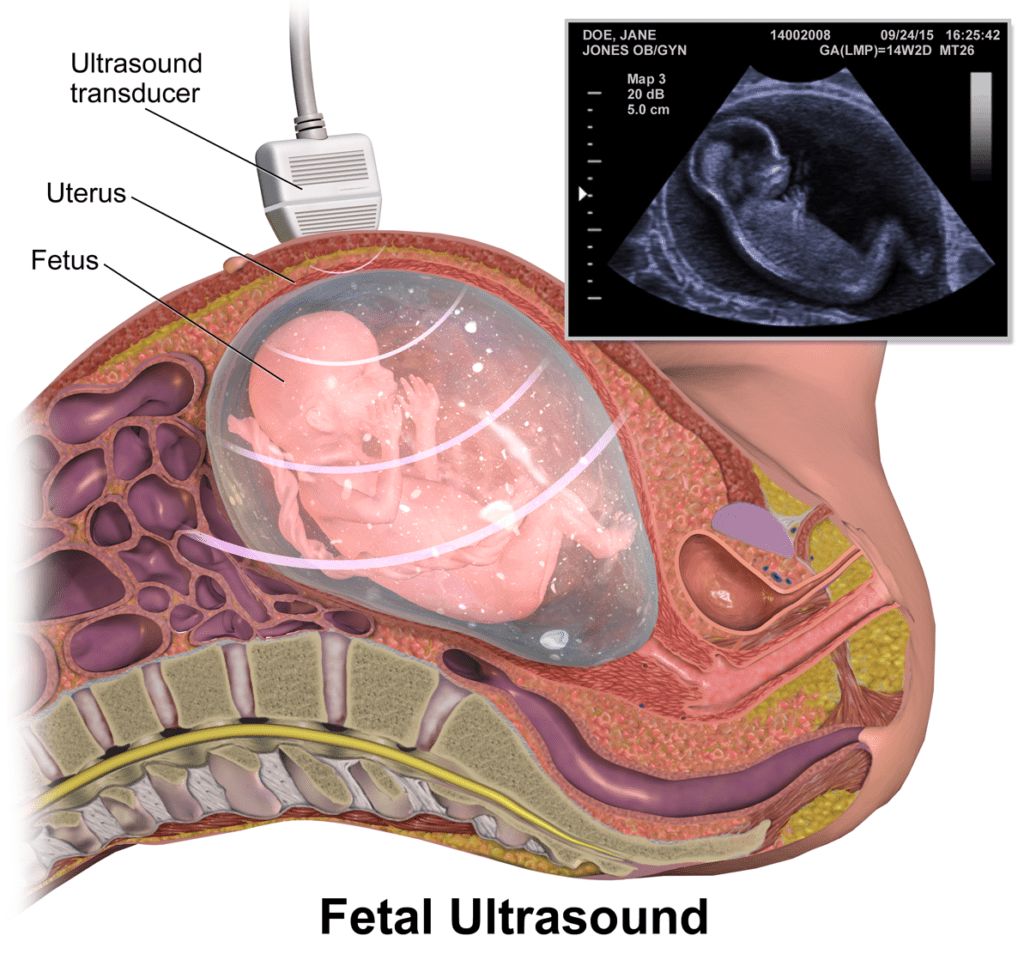
What are ultrasounds used for?
In general, ultrasounds are used to image internal organs. They are used during pregnancy to achieve images of the fetus. Cranial ultrasounds are often performed on newborns in the NICU to produce useful images of the brain and surrounding areas. Ultrasounds are valuable for identifying cerebral edema and parenchymal or intraventricular hemorrhage (8).
Preparing for neonatal ultrasounds
Usually no special preparation is required for an infant to get an ultrasound. As with the other imaging methods, however, a physician may recommend that the infant receive an anesthetic before getting an ultrasound. Ultrasounds tend to be much less invasive than MRIs and CTs because the infant can stay in their crib or incubator in the NICU for the procedure and the imaging is done in one small area instead of involving the entire body. It is important to note that often cranial ultrasounds and MRIs are used together to produce complete and progressive images of newborns in the NICU (8).
Benefits of ultrasound
- No radiation
- Mobile, easily used within the NICU
- Suitable for 1 to 2 scans per day
Limitations of ultrasound
- Produces a less clear and complete picture than other available technologies
- Difficult to pinpoint exact location of certain injuries
- Requires absolute expertise of the ultrasound administrator and interpreter
- Is capable of producing some biological effects in the body under certain conditions and settings, such as producing small pockets of gas in tissues or bodily fluids or heating the tissues in the body.
- Ultrasound should only be used, especially on neonates, if medically necessary (9).
Can you request neonatal imaging?
If you have a concern about your infant, always discuss it with your doctor. Normally doctors will recommend imaging tests when certain concerns arise, but you have the right to ask about imaging options at any time. If your doctor recommends imaging and you would like more information on any imaging technique or decision, don’t hesitate to ask your physician. Frequently, after a baby comes back from the NICU, follow-up imaging isn’t done unless a parent insists on it. Don’t be afraid to insist on getting follow-up imaging done, as these tests can provide highly valuable information regarding your child’s development.
Takeaways: Neonatal imaging
While the MRI is more expensive, it is most highly recommended due to its ability to produce a clear image and its lack of ionizing radiation. Your physician will provide you with information on the appropriate or suggested imaging procedures, and from here a decision can be made.


About ABC Law Centers
ABC Law Centers was established to focus exclusively on birth injury cases. A “birth injury” is any type of harm to a baby that occurs just before, during, or after birth. This includes issues such as oxygen deprivation, infection, and trauma. While some children with birth injuries make a complete recovery, others develop disabilities such as cerebral palsy, hypoxic-ischemic encephalopathy, epilepsy and others.
It is considered medical malpractice if a birth injury or a related disability could have been prevented with proper care. Your child could have their lifelong treatment, care, and other crucial resources covered by a birth injury case settlement.
If you believe you may have a birth injury case for your child, please contact us today to learn more. We are happy to hear your story and answer your questions free of any obligation or charge, even if you decide not to pursue a legal case with us. If you do, you would pay nothing throughout the entire legal process unless we win.
- Free Case Review
- Available 24/7
- No Fee Unless We Win
Featured Videos
Posterior Position
Hypoxic-Ischemic Encephalopathy (HIE)

Featured Testimonial
What Our
Clients Say…
After the traumatic birth of my son, I was left confused, afraid, and seeking answers. We needed someone we could trust and depend on. ABC Law Centers was just that.
- Michael
Helpful resources
- Magnetic Resonance Imaging (MRI). (2018, July 17). Retrieved October 20, 2018, from https://www.nibib.nih.gov/science-education/science-topics/magnetic-resonance-imaging-mri
- Magnetic Resonance Imaging (MRI) | Boston Children’s Hospital. (n.d.). Retrieved October 20, 2018, from http://www.childrenshospital.org/conditions-and-treatments/treatments/mri
- Diagnosis of Infant Seizures. (2013, August 27). Retrieved October 20, 2018, from https://www.epilepsy.com/living-epilepsy/parents-and-caregivers/about-newborns-and-infants/diagnosis-infant-seizures
- Dowshen, S. (Ed.). (2014, March). Magnetic Resonance Imaging (MRI). Retrieved October 20, 2018, from https://kidshealth.org/en/parents/mri.html
- Radiological Society of North America, RSNA, & American College of Radiology. (n.d.). Children’s (Pediatric) Magnetic Resonance Imaging. Retrieved October 20, 2018, from https://www.radiologyinfo.org/en/info.cfm?pg=pediatric-mri
- CT scan. (2018, May 09). Retrieved October 20, 2018, from https://www.mayoclinic.org/tests-procedures/ct-scan/about/pac-20393675
- Radiological Society of North America, RSNA, & American College of Radiology. (n.d.). Children’s (Pediatric) CT (Computed Tomography). Retrieved October 20, 2018, from https://www.radiologyinfo.org/en/info.cfm?pg=pedia-ct
- Ultrasound. (2017, November 20). Retrieved October 20, 2018, from https://www.nibib.nih.gov/science-education/science-topics/ultrasound
- Center for Devices and Radiological Health. (n.d.). Medical Imaging – Ultrasound Imaging. Retrieved October 22, 2018, from https://www.fda.gov/radiation-emittingproducts/radiationemittingproductsandprocedures/medicalimaging/ucm115357.htm