What types of brain bleeds are there? What causes each type of brain bleed?
An intracranial hemorrhage (brain bleed) is a traumatic or hypoxic birth injury characterized by sudden, rapid bleeding within the infant’s skull or brain. Extracranial hemorrhages, which are similar to intracranial hemorrhages, are characterized by bleeding just outside the skull. Causes and risk factors for brain bleeds vary depending on the type and location of the brain bleed. Common risk factors and causes for infant intracranial hemorrhages include misuse of vacuum extractors and/or forceps, delayed or prolonged delivery, premature birth, umbilical cord complications, and size incompatibilities between the fetus and mother’s birth canal. Throughout this page, we’ll cover the specific causes of different types of neonatal brain bleeds, including subarachnoid hemorrhages, subdural hemorrhages, intraventricular hemorrhages, germinal matrix hemorrhages, subgaleal hemorrhages, and cephalohematomas.
Types of Intracranial Hemorrhages (Brain Bleeds) and Their Causes
I. Subarachnoid Hemorrhage (SAH) and Subdural Hemorrhage (SDH)
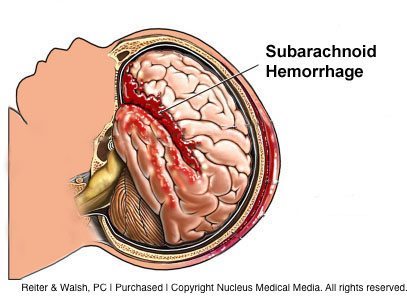 Subarachnoid hemorrhage (SAH) is the second most commonly detected neonatal brain bleed and is caused by rupture of veins in the space or spaces near the skull. Hydrocephalus (fluid in the brain) can develop after a subarachnoid hemorrhage because the bleeding causes too much cerebral spinal fluid (CSF) to build up in the brain’s ventricles, which can cause brain and head swelling. Subarachnoid hemorrhage can also cause oxygen to be cut off in certain parts of the brain, which can cause brain tissue to die. This can cause permanent brain damage, such as cerebral palsy and periventricular leukomalacia (PVL).
Subarachnoid hemorrhage (SAH) is the second most commonly detected neonatal brain bleed and is caused by rupture of veins in the space or spaces near the skull. Hydrocephalus (fluid in the brain) can develop after a subarachnoid hemorrhage because the bleeding causes too much cerebral spinal fluid (CSF) to build up in the brain’s ventricles, which can cause brain and head swelling. Subarachnoid hemorrhage can also cause oxygen to be cut off in certain parts of the brain, which can cause brain tissue to die. This can cause permanent brain damage, such as cerebral palsy and periventricular leukomalacia (PVL).
Subdural hemorrhage (SDH) or hematoma, is the most common type of brain bleed in newborns. Subdural hemorrhage occurs when there is rupture of the blood vessels in the area between the surface of the brain and the thin layer of tissue that separates the brain from the skull. Sometimes subdural hemorrhage causes an increase in pressure inside the brain, which can cause an increase in head size, apnea (periods of not breathing), bradycardia (slow heart rate), and coma.
Signs and symptoms of subarachnoid hemorrhage and subdural hemorrhage include:
- Shallow breathing
- Difficulty breathing
- Apnea
- Neonatal seizures
- Irritability
- Altered muscle tone
- Altered level of consciousness
Causes of and risk factors for subarachnoid hemorrhage and subdural hemorrhage include the following:
- Use of forceps or vacuum extractors to facilitate delivery
- A vaginal delivery when the baby is in breech presentation. Research shows that a C-section delivery is the safest way to deliver babies in this position.
- Improperly managed face or brow presentation
- Macrosomia (larger than average baby)
- Cephalopelvic disproportion (the baby’s head is too large to easily pass through the mother’s pelvis)
- Precipitous delivery, which is characterized by a very fast delivery, often accompanied by strong contractions. Drugs used to start or speed up labor and delivery, such as Pitocin (oxytocin) and Cytotec, can cause contractions that are so fast and strong that they deprive the baby of oxygen. Sometimes strong contractions can also cause head trauma.
- Prolonged labor and delivery, which can be very traumatic for an infant. This can occur when a baby is very large, when the baby is not in the normal position in the birth canal (for example, breech, face, or brow presentation), and when the mother’s pelvis is too small for the baby. Many conditions can cause prolonged labor, and oftentimes, physicians fail to move on to C-section delivery when it is medically necessary. During the extended vaginal labor and attempted delivery, the physician may use Pitocin or Cytotec to try and speed up delivery, or vacuum extractors and forceps may be used to try and facilitate delivery. All of these actions can cause a traumatic injury to the head with resultant brain bleeding.
II. Intraventricular Hemorrhage (IVH)
 The brain has four ventricles in the middle of it. Intraventricular hemorrhage is a type of brain bleed characterized by bleeding inside the brain’s ventricles. Intraventricular hemorrhage is most common in preterm babies, although term babies can have IVH as well. Premature babies are more susceptible to intraventricular hemorrhage because blood vessels and other parts of their brains are fragile.
The brain has four ventricles in the middle of it. Intraventricular hemorrhage is a type of brain bleed characterized by bleeding inside the brain’s ventricles. Intraventricular hemorrhage is most common in preterm babies, although term babies can have IVH as well. Premature babies are more susceptible to intraventricular hemorrhage because blood vessels and other parts of their brains are fragile.
Signs and symptoms of IVH include the following:
- Irritability
- Neonatal seizures
- Apnea
- Bulging fontanelle (soft spot)
Intraventricular hemorrhage can be caused by the same factors that cause subarachnoid hemorrhage and subdural hemorrhage, which are listed above. IVH can also be caused by oxygen deprivation in the baby’s brain, which is a dangerous condition known as hypoxia. Thus, any conditions that cause hypoxia can also cause intraventricular hemorrhage. Some of these conditions, injuries, and complications include the following:
-
- Nuchal cord
- Uterine rupture
- Placental abruption
- Delayed delivery
- Prolonged labor
- Misuse of Pitocin or Cytotec
- Preeclampsia
-
- Hypoxic-ischemic encephalopathy (HIE): Hypoxic-ischemic encephalopathy is brain injury caused by a lack of oxygen to the brain due to low oxygen in the blood or lack of blood flow in the brain
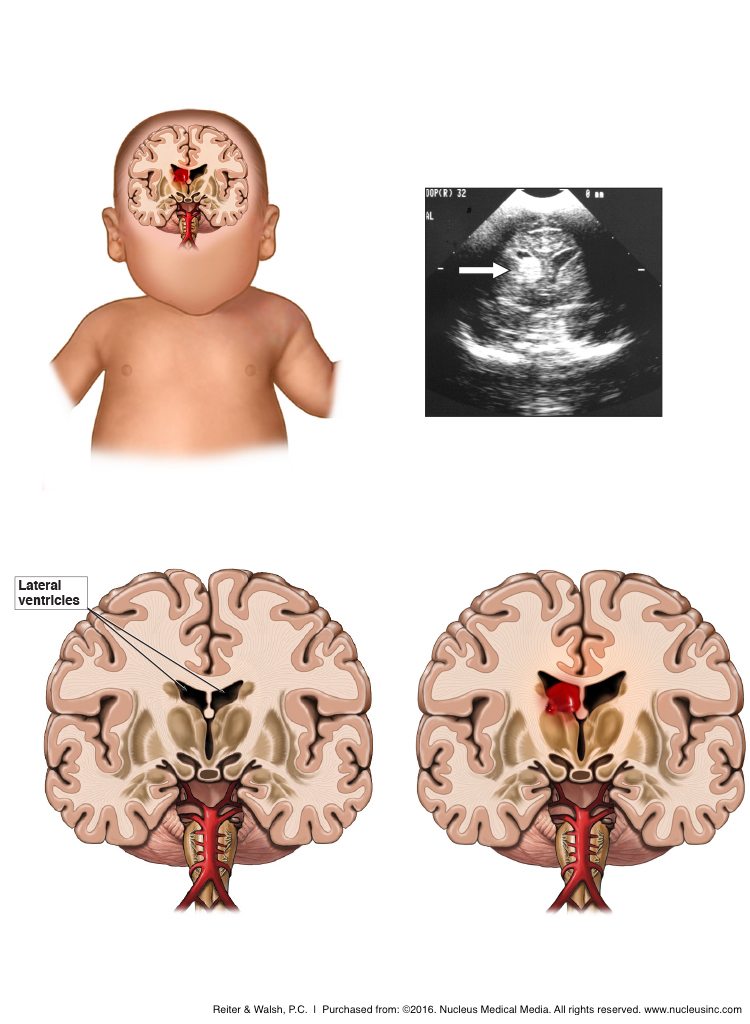
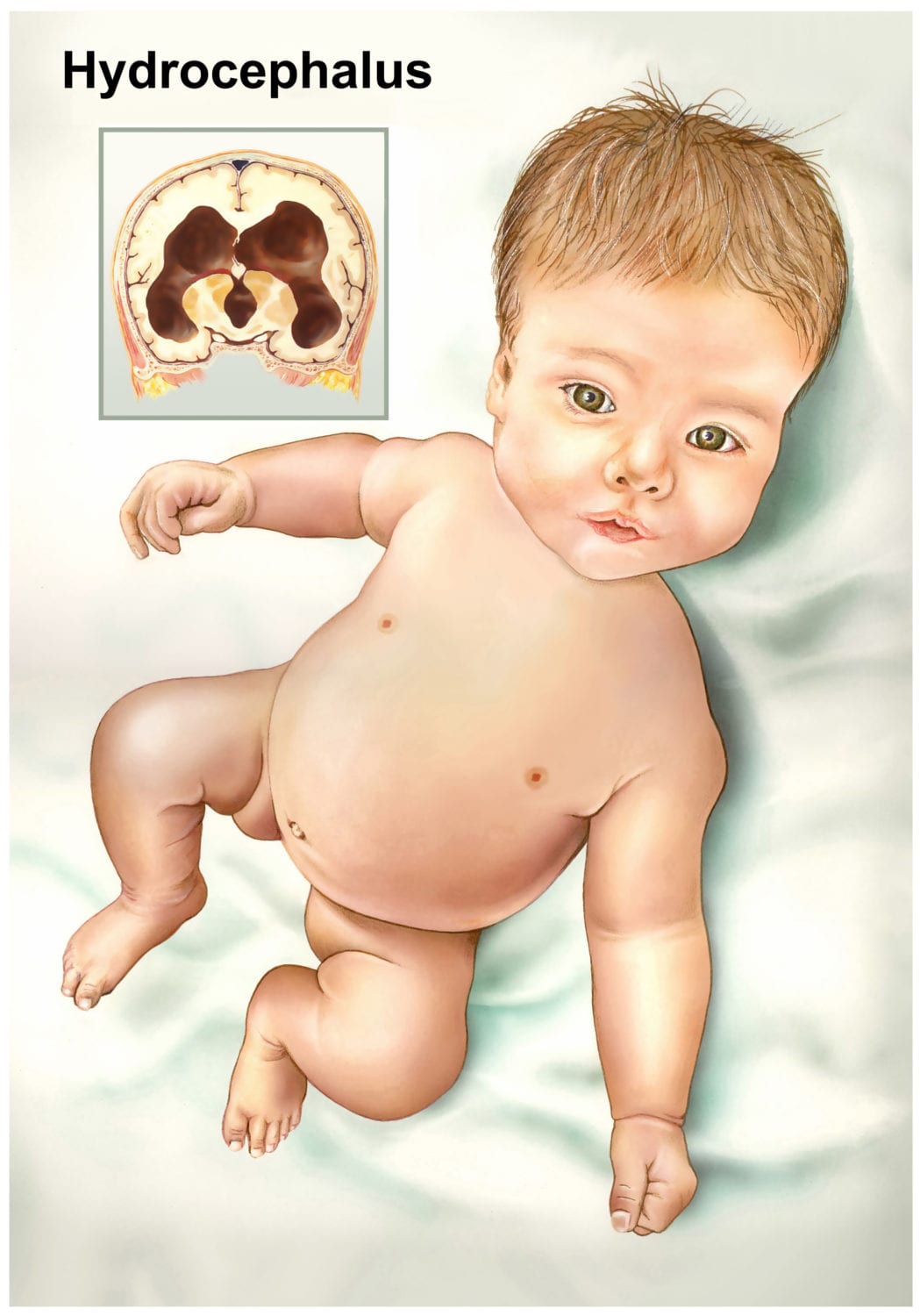 Very close monitoring of infants with IVH is crucial due to the potential for the bleeding to extend into the tissue around it and cause hydrocephalus and permanent brain damage. The most common cause of hydrocephalus is a germinal matrix hemorrhage (GMH). GMH occurs primarily in premature infants. This is because activity in the germinal matrix peaks at 8-23 weeks of gestation. The germinal matrix helps create the fully-formed brain; cells develop and leave this structure during brain development. Damage to the germinal matrix at weeks 8-23 can cause severe brain damage and death. A GMH occurs when there is bleeding into the part of the germinal matrix that is connected to the ventricles. When this occurs, there may be subsequent rupture into the ventricles. A GMH causes the ventricles to be filled with blood and cellular products, and this, among other things, causes dilation of the ventricles. GMH leads to a lot of stress on the areas around it, as well as congestion of the blood vessels. All of these factors can cause injury to the very important white matter in the brain.
Very close monitoring of infants with IVH is crucial due to the potential for the bleeding to extend into the tissue around it and cause hydrocephalus and permanent brain damage. The most common cause of hydrocephalus is a germinal matrix hemorrhage (GMH). GMH occurs primarily in premature infants. This is because activity in the germinal matrix peaks at 8-23 weeks of gestation. The germinal matrix helps create the fully-formed brain; cells develop and leave this structure during brain development. Damage to the germinal matrix at weeks 8-23 can cause severe brain damage and death. A GMH occurs when there is bleeding into the part of the germinal matrix that is connected to the ventricles. When this occurs, there may be subsequent rupture into the ventricles. A GMH causes the ventricles to be filled with blood and cellular products, and this, among other things, causes dilation of the ventricles. GMH leads to a lot of stress on the areas around it, as well as congestion of the blood vessels. All of these factors can cause injury to the very important white matter in the brain.
III. Subgaleal Hemorrhage
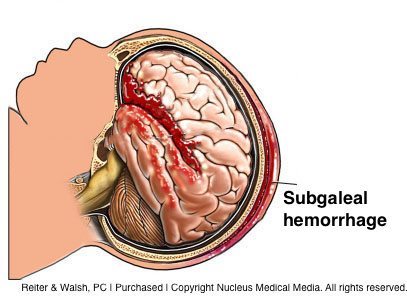 A subgaleal hemorrhage is a potentially deadly type of brain bleed. Subgaleal hemorrhages are strongly associated with birth trauma and delivery using forceps and vacuum extractors, with vacuum extraction being the greatest risk factor. A subgaleal hemorrhage is caused by rupture of veins that are very close to the scalp. When these veins rupture, blood builds up just beneath the scalp, and the baby will have swelling of the head and evidence of shock, which is characterized by severely low blood volume and blood pressure. Prompt and aggressive treatment is critical when this occurs. Treatment for a subgaleal hemorrhage includes administration of blood products to help increase blood pressure. The sooner treatment of a subgaleal hemorrhage occurs, the better the outcome for the baby. Subgaleal hemorrhages can lead to epilepsy, cerebral palsy, severe hearing problems, and death.
A subgaleal hemorrhage is a potentially deadly type of brain bleed. Subgaleal hemorrhages are strongly associated with birth trauma and delivery using forceps and vacuum extractors, with vacuum extraction being the greatest risk factor. A subgaleal hemorrhage is caused by rupture of veins that are very close to the scalp. When these veins rupture, blood builds up just beneath the scalp, and the baby will have swelling of the head and evidence of shock, which is characterized by severely low blood volume and blood pressure. Prompt and aggressive treatment is critical when this occurs. Treatment for a subgaleal hemorrhage includes administration of blood products to help increase blood pressure. The sooner treatment of a subgaleal hemorrhage occurs, the better the outcome for the baby. Subgaleal hemorrhages can lead to epilepsy, cerebral palsy, severe hearing problems, and death.
IV. Cephalohematoma (Cephalhematoma)
A cephalohematoma (or cephalhematoma) is a brain bleed in which blood collects between the skull and its covering as the result of ruptured vessels. Cephalohematoma can be caused by any type of trauma to the baby’s head, but it is most commonly associated with forceps and vacuum extraction delivery. The swelling does not cross suture lines, which are bands of tissue that connect the bones of the skull. Discoloration may or may not be present, and there typically isn’t significant blood loss. However, if a cephalohematoma is left unresolved, calcification of the hematoma can occur, which will cause a bony swelling that can last for months. This can cause skull deformities in the baby, which often require surgery. Untreated cephalohematoma also can lead to severe infection in the baby, which can cause pus-filled formations and death of parts of the skull.
Legal Help for Intracranial Hemorrhages
Trusted Birth Trauma Attorneys Representing Brain Bleed Victims
Several instances of medical malpractice can lead to a neonatal brain bleed diagnosis. Medical professionals are held to high standards when caring for mothers and their babies during the fragile processes of pregnancy, labor, and delivery. Any medical error or deviation from medical care standards is considered medical negligence. If your loved one suffered a brain bleed around the time of delivery that you attribute to an act of negligence, we encourage you to reach out to our birth trauma team for a free legal consultation. Reiter & Walsh, P.C. is one of the only firms in the country specifically and exclusively handling birth injury cases. Every day, our birth trauma attorneys help families like yours secure the resources they need to live lives of rehabilitation, well-being, and equal opportunity. To start your free case review, you may contact us in any of the following ways:
Free Case Review | Available 24/7 | No Fee Until We Win
Call our toll-free phone line at 888-419-2229
Press the Live Chat button on your browser
Complete Our Online Contact Form