If I experience bleeding during pregnancy, could it hurt my baby?
Disclaimer: Please know that our website is owned by a law firm that focuses exclusively on birth injury cases. We try to provide useful medical information to our readers, but we cannot provide treatments or medical advice. If you might be having a medical emergency, please call 911 (or your country’s emergency number) and seek immediate medical attention.
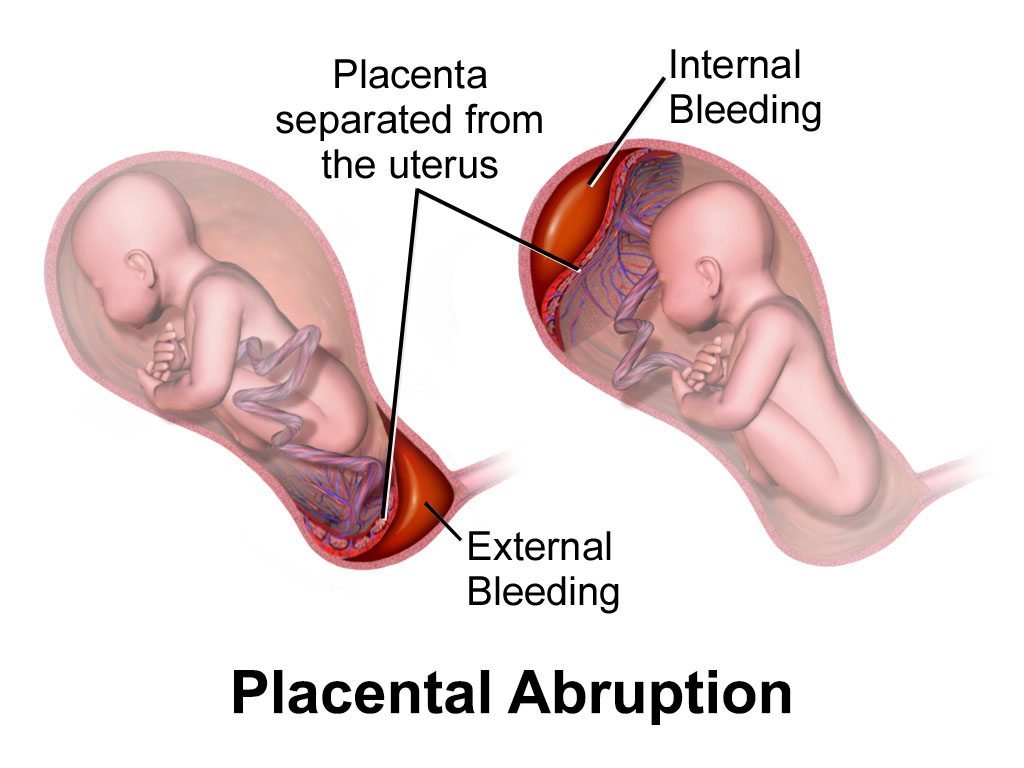
Yes, bleeding during pregnancy may cause injury to the baby. Bleeding during pregnancy could be caused by a number of things (1). One very serious condition that can cause bleeding is placental abruption (though abruption can also occur without visible bleeding). The placenta is an organ that connects the baby to the wall of the womb (uterus). Some of the placenta’s important functions include delivering nutrients and oxygen to the baby. Nutrients and oxygen travel from the mother to the placenta, and then through the umbilical cord to the baby. A placental abruption occurs when the placenta separates from the womb. The separation can be partial or complete. If the separation is complete, the baby will be totally cut off from the mother’s circulation and will therefore not be receiving any nutrients or oxygen, nor will the baby be able to get rid of waste products, such as carbon dioxide (2, 3).
Risk factors for placental abruption
If a woman has risk factors for placental abruption, medical professionals should be monitoring and administering care accordingly. Risk factors for placental abruption include, but are not limited to (2,3):
- Preeclampsia or high blood pressure. This is the most common cause of placental abruption, occurring in about 44% of cases.
- Trauma or contractions during labor
- Labor induction drugs such as Pitocin and Cytotec increase the risk of placental abruption because they cause uterine tachysystole (a complication in which contractions are stronger, more frequent, or longer-lasting; this can cause the placenta to tear away from the uterus).
- Sudden decompression of the uterus from events such as the delivery of the first child in a multiples birth or premature rupture of membranes (mother’s water breaking too soon)
- Accidental puncture of the placenta from a needle (e.g. amniocentesis)
- Chorioamnionitis (an infection of the two membranes of the placenta – the chorion and the amnion – and the amniotic fluid.)
- Abnormal uterine blood vessels
- Previous placental abruption
- Mother over the age of 35 or younger than 20
- Male baby
Signs of placental abruption
Signs of placental abruption include (3):
- Bleeding during the second half of pregnancy or excessive bleeding during labor
- Mild or intense abdominal pain
- Back pain
- Uterine contractions during labor that last longer than normal
- Uterine irritability
- Uterus that becomes hard to the touch during labor
- Disproportionately enlarged uterus
- Identification of bleeding behind the placenta (retroplacental hematoma) on ultrasound
- Debris in the amniotic fluid, thickened placenta, and collection of fluid around the maternal-fetal membranes on ultrasound
- Blood tests, such as a fibrinogen level and DIC, can help reveal the degree of abruption and bleeding.
- Maternal low blood pressure (hypotension) and fetal heart rate abnormalities suggest significant placental separation that could result in severe oxygen deprivation or death.
Small amounts of bleeding can signal a larger problem
Bleeding can be concealed and therefore not escape through the vagina; thus, when abdominal pain and uterine contractions are present, a patient should be carefully evaluated for abruption even if there is minimal or no vaginal bleeding.
Trusted legal help for maternal bleeding, placental abruption, and birth injury
If you are seeking the help of a placental abruption attorney, it is very important to choose a lawyer and firm that focuses solely on birth injury cases. ABC Law Centers (Reiter & Walsh, P.C.) is a national birth injury law firm that has been helping children for over three decades.
Our firm has numerous multi-million dollar verdicts and settlements that attest to our success, and you pay nothing until we win your case. Email or call us at 248-593-5100 for a free case evaluation. We do not charge any fees for the entire legal process unless we win. Our firm’s award-winning lawyers are available 24 / 7 to speak with you.
Related resources
- Bleeding During Pregnancy: An Overview of Maternal Bleeding Throughout Pregnancy and Delivery
- Placental Abruption
- Birth Injury Glossary
- Our Verdicts and Settlements
Sources
- Bleeding During Pregnancy and Birth: Risks to the Baby. (n.d.). Retrieved June 3, 2020, from https://www.abclawcenters.com/practice-areas/prenatal-birth-injuriesmaternal-medical-conditionsbleeding-during-pregnancy-delivery/
- Placental Abruption: Risks, Causes, Symptoms and Treatment. (2017, May 02). Retrieved February 18, 2019, from http://americanpregnancy.org/pregnancy-complications/placental-abruption/
- Placental Abruption: Danger to Mothers and Babies. (n.d.). Retrieved June 3, 2020, from https://www.abclawcenters.com/practice-areas/prenatal-birth-injuries/labor-and-delivery-complications-and-errors/placental-abruption/